As US hospitals make the necessary shuffle to accommodate the current wave, I would like to remind leadership about the study done on the psychological status of frontline hospital workers during NYC's spring Covid surge (thread).
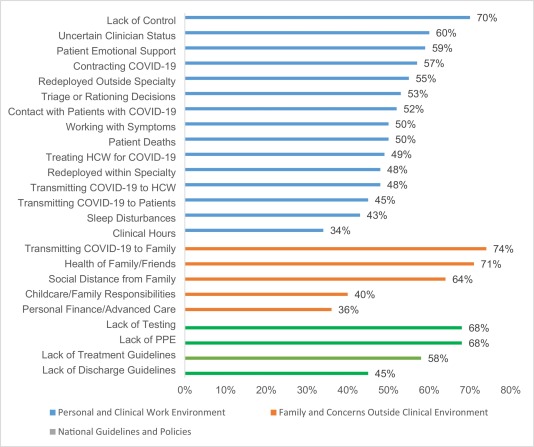
- Perceptions of a lack of control and/or uncertainty
- Performing clinical work that is outside of your specialty
- The need/expectation for healthcare providers to provide social support to patients in lieu of their families (due to visitation restrictions)
- And also fears related to getting/transmitting Covid within the work environment - in particular, the uncertain Covid status of other healthcare providers
More from Health
You gotta think about this one carefully!
Imagine you go to the doctor and get tested for a rare disease (only 1 in 10,000 people get it.)
The test is 99% effective in detecting both sick and healthy people.
Your test comes back positive.
Are you really sick? Explain below 👇
The most complete answer from every reply so far is from Dr. Lena. Thanks for taking the time and going through
You can get the answer using Bayes' theorem, but let's try to come up with it in a different —maybe more intuitive— way.
👇
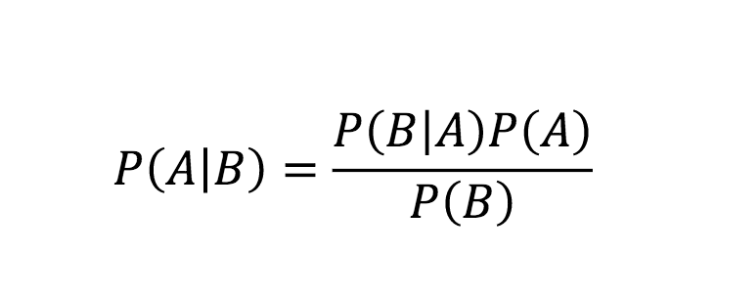
Here is what we know:
- Out of 10,000 people, 1 is sick
- Out of 100 sick people, 99 test positive
- Out of 100 healthy people, 99 test negative
Assuming 1 million people take the test (including you):
- 100 of them are sick
- 999,900 of them are healthy
👇
Let's now test both groups, starting with the 100 people sick:
▫️ 99 of them will be diagnosed (correctly) as sick (99%)
▫️ 1 of them is going to be diagnosed (incorrectly) as healthy (1%)
👇
Imagine you go to the doctor and get tested for a rare disease (only 1 in 10,000 people get it.)
The test is 99% effective in detecting both sick and healthy people.
Your test comes back positive.
Are you really sick? Explain below 👇
The most complete answer from every reply so far is from Dr. Lena. Thanks for taking the time and going through
Really doesn\u2019t fit well in a tweet. pic.twitter.com/xN0pAyniFS
— Dr. Lena Sugar \U0001f3f3\ufe0f\u200d\U0001f308\U0001f1ea\U0001f1fa\U0001f1ef\U0001f1f5 (@_jvs) February 18, 2021
You can get the answer using Bayes' theorem, but let's try to come up with it in a different —maybe more intuitive— way.
👇
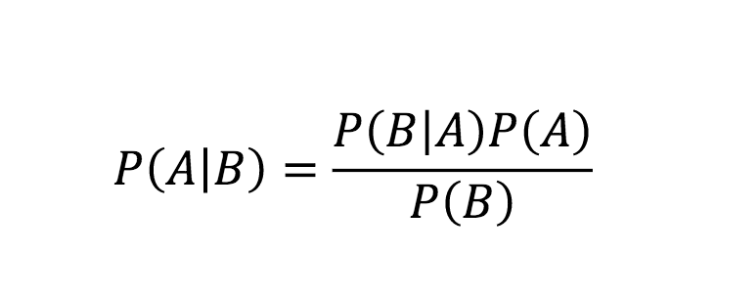
Here is what we know:
- Out of 10,000 people, 1 is sick
- Out of 100 sick people, 99 test positive
- Out of 100 healthy people, 99 test negative
Assuming 1 million people take the test (including you):
- 100 of them are sick
- 999,900 of them are healthy
👇
Let's now test both groups, starting with the 100 people sick:
▫️ 99 of them will be diagnosed (correctly) as sick (99%)
▫️ 1 of them is going to be diagnosed (incorrectly) as healthy (1%)
👇
Thread on how atheism leads to mental retardation (backed with medical citations🧵💉)
To start with, atheism is an unnatural self-contradicting doctrine.
Medical terminology proves that human beings are naturally pre-disposed to believe in God. Oxford scientists assert that people are "born believers".
https://t.co/kE0Fi588yn
https://t.co/OqyXcGIMJn

It should be known that atheism could never produce an intelligently-functioning society and neither ever will.
Contrastingly, Islam produced several intellectuals & polymaths, was on the forefront of scientific development, boasting 100% literacy
It is also scientifically proven that atheism led to lesser scientific curiosity and scientific frauds, which is also why atheists incline to pseudo-science.
Whereas, religion in general and Islam in particular boosted education.
https://t.co/19Onc84u3g

Atheists are also likely to affected by pervasive mental and developmental disorders like high-functioning autism.
Cognitive Scientists and renowned Neurologists found that more atheism is leads to greater autism.
https://t.co/zRjEyFoX3P

To start with, atheism is an unnatural self-contradicting doctrine.
Medical terminology proves that human beings are naturally pre-disposed to believe in God. Oxford scientists assert that people are "born believers".
https://t.co/kE0Fi588yn
https://t.co/OqyXcGIMJn

It should be known that atheism could never produce an intelligently-functioning society and neither ever will.
Contrastingly, Islam produced several intellectuals & polymaths, was on the forefront of scientific development, boasting 100% literacy
If the Muslim world had not existed, there literally would be no technology/achievements today.
— Starks\u262a\ufe0f\U0001f1f9\U0001f1e9 (@MegaIntelIect) January 8, 2021
Science only developed because of Islam, Europe should be grateful to Islam for civilizing their barbaric cult.
Source: The Caliph's Splendor, Pg 204-05 https://t.co/HVypO52Tpc pic.twitter.com/00jYSbaDSs
It is also scientifically proven that atheism led to lesser scientific curiosity and scientific frauds, which is also why atheists incline to pseudo-science.
Whereas, religion in general and Islam in particular boosted education.
https://t.co/19Onc84u3g

Atheists are also likely to affected by pervasive mental and developmental disorders like high-functioning autism.
Cognitive Scientists and renowned Neurologists found that more atheism is leads to greater autism.
https://t.co/zRjEyFoX3P

You May Also Like
BREAKING: @CommonsCMS @DamianCollins just released previously sealed #Six4Three @Facebook documents:
Some random interesting tidbits:
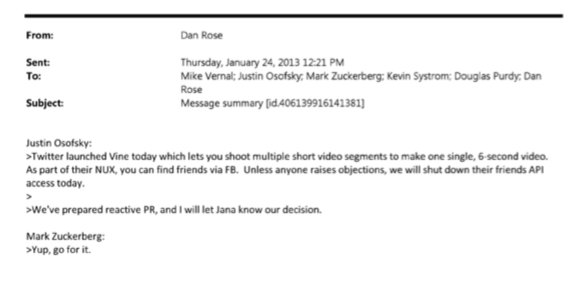
1) Zuck approves shutting down platform API access for Twitter's when Vine is released #competition
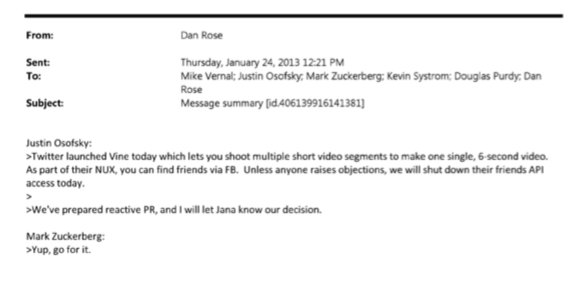
2) Facebook engineered ways to access user's call history w/o alerting users:
Team considered access to call history considered 'high PR risk' but 'growth team will charge ahead'. @Facebook created upgrade path to access data w/o subjecting users to Android permissions dialogue.
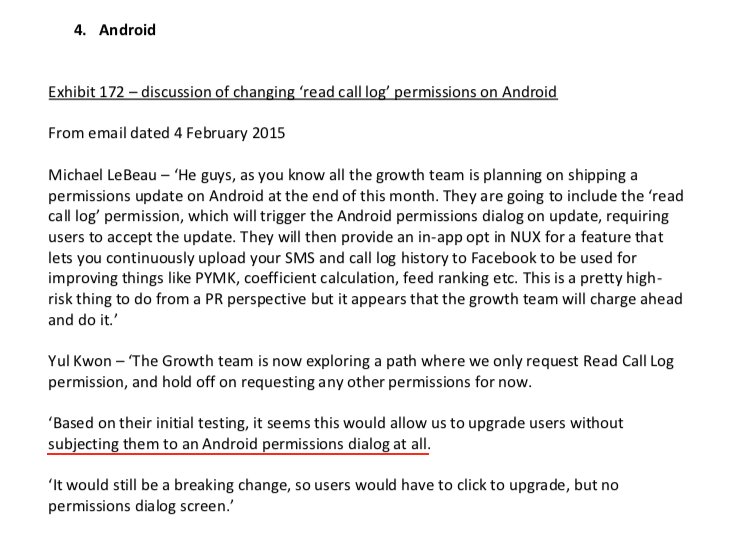
3) The above also confirms @kashhill and other's suspicion that call history was used to improve PYMK (People You May Know) suggestions and newsfeed rankings.
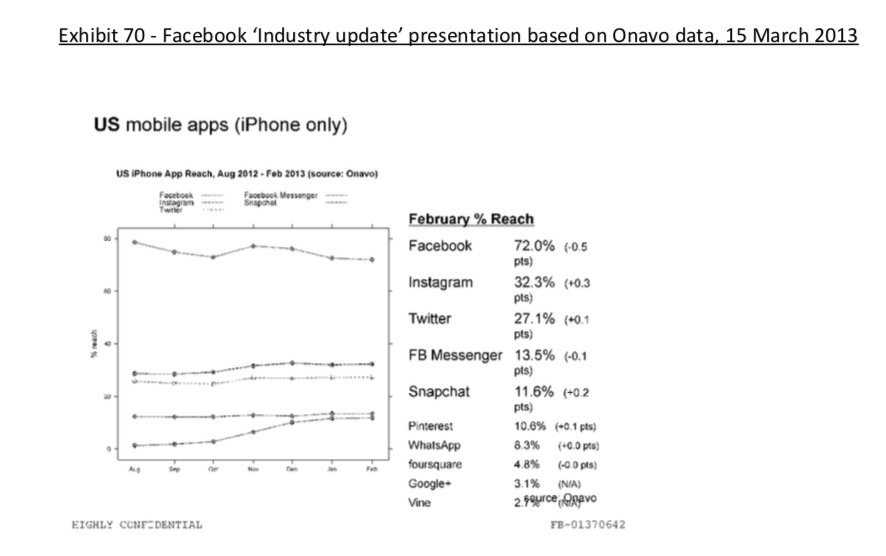
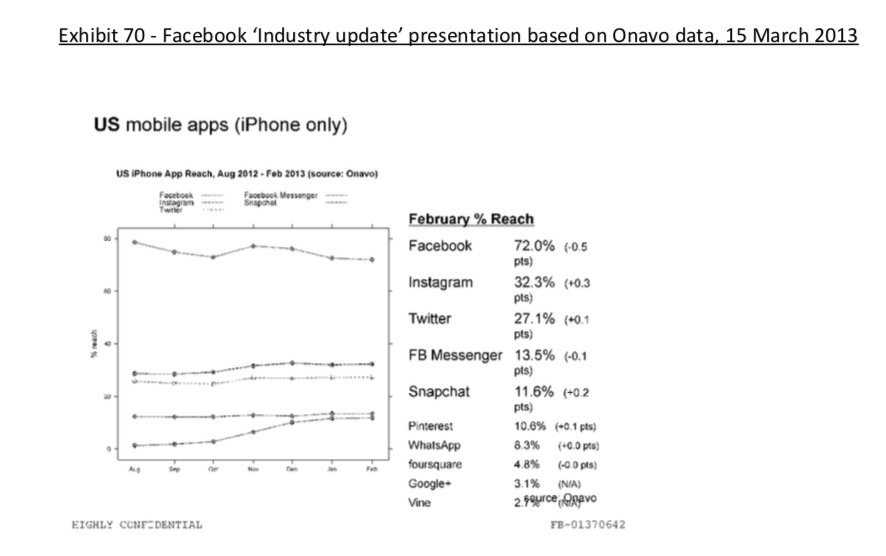
4) Docs also shed more light into @dseetharaman's story on @Facebook monitoring users' @Onavo VPN activity to determine what competitors to mimic or acquire in 2013.
https://t.co/PwiRIL3v9x
Some random interesting tidbits:
1) Zuck approves shutting down platform API access for Twitter's when Vine is released #competition
2) Facebook engineered ways to access user's call history w/o alerting users:
Team considered access to call history considered 'high PR risk' but 'growth team will charge ahead'. @Facebook created upgrade path to access data w/o subjecting users to Android permissions dialogue.
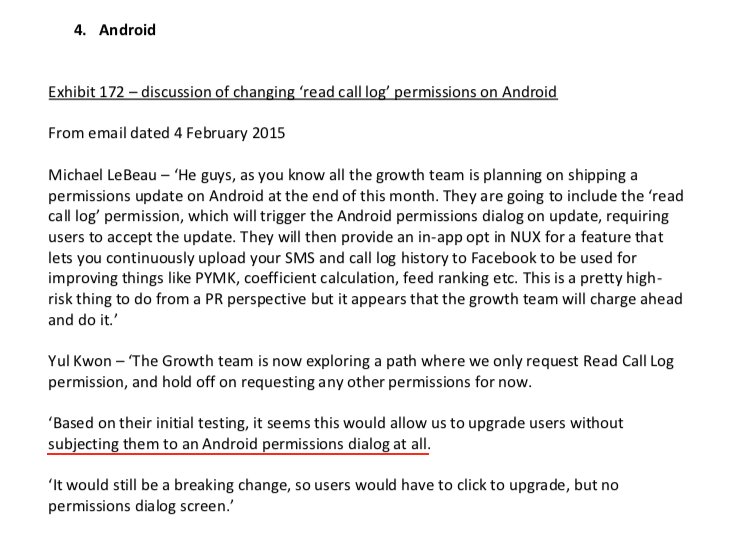
3) The above also confirms @kashhill and other's suspicion that call history was used to improve PYMK (People You May Know) suggestions and newsfeed rankings.
4) Docs also shed more light into @dseetharaman's story on @Facebook monitoring users' @Onavo VPN activity to determine what competitors to mimic or acquire in 2013.
https://t.co/PwiRIL3v9x
Nano Course On Python For Trading
==========================
Module 1
Python makes it very easy to analyze and visualize time series data when you’re a beginner. It's easier when you don't have to install python on your PC (that's why it's a nano course, you'll learn python...
... on the go). You will not be required to install python in your PC but you will be using an amazing python editor, Google Colab Visit https://t.co/EZt0agsdlV
This course is for anyone out there who is confused, frustrated, and just wants this python/finance thing to work!
In Module 1 of this Nano course, we will learn about :
# Using Google Colab
# Importing libraries
# Making a Random Time Series of Black Field Research Stock (fictional)
# Using Google Colab
Intro link is here on YT: https://t.co/MqMSDBaQri
Create a new Notebook at https://t.co/EZt0agsdlV and name it AnythingOfYourChoice.ipynb
You got your notebook ready and now the game is on!
You can add code in these cells and add as many cells as you want
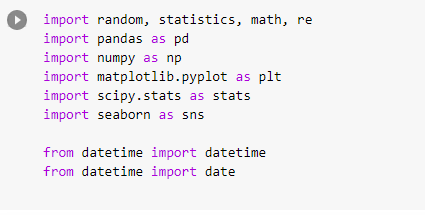
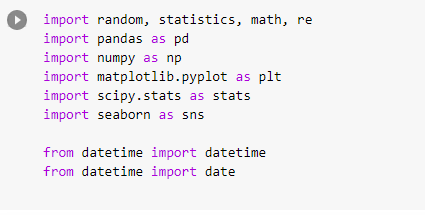
# Importing Libraries
Imports are pretty standard, with a few exceptions.
For the most part, you can import your libraries by running the import.
Type this in the first cell you see. You need not worry about what each of these does, we will understand it later.
==========================
Module 1
Python makes it very easy to analyze and visualize time series data when you’re a beginner. It's easier when you don't have to install python on your PC (that's why it's a nano course, you'll learn python...
... on the go). You will not be required to install python in your PC but you will be using an amazing python editor, Google Colab Visit https://t.co/EZt0agsdlV
This course is for anyone out there who is confused, frustrated, and just wants this python/finance thing to work!
In Module 1 of this Nano course, we will learn about :
# Using Google Colab
# Importing libraries
# Making a Random Time Series of Black Field Research Stock (fictional)
# Using Google Colab
Intro link is here on YT: https://t.co/MqMSDBaQri
Create a new Notebook at https://t.co/EZt0agsdlV and name it AnythingOfYourChoice.ipynb
You got your notebook ready and now the game is on!
You can add code in these cells and add as many cells as you want
# Importing Libraries
Imports are pretty standard, with a few exceptions.
For the most part, you can import your libraries by running the import.
Type this in the first cell you see. You need not worry about what each of these does, we will understand it later.