The problem with meta-analysis like this is that it obfuscates the most important issue of treatment, which is timing.
#BMJResearch update: Corticosteroids probably reduce mortality and mechanical ventilation in patients with covid-19 compared with standard care, whereas azithromycin, hydroxychloroquine, interferon-beta, and tocilizumab may not reduce either https://t.co/oQ3lTWUqaz
— The BMJ (@bmj_latest) December 18, 2020
More from Robin Monotti
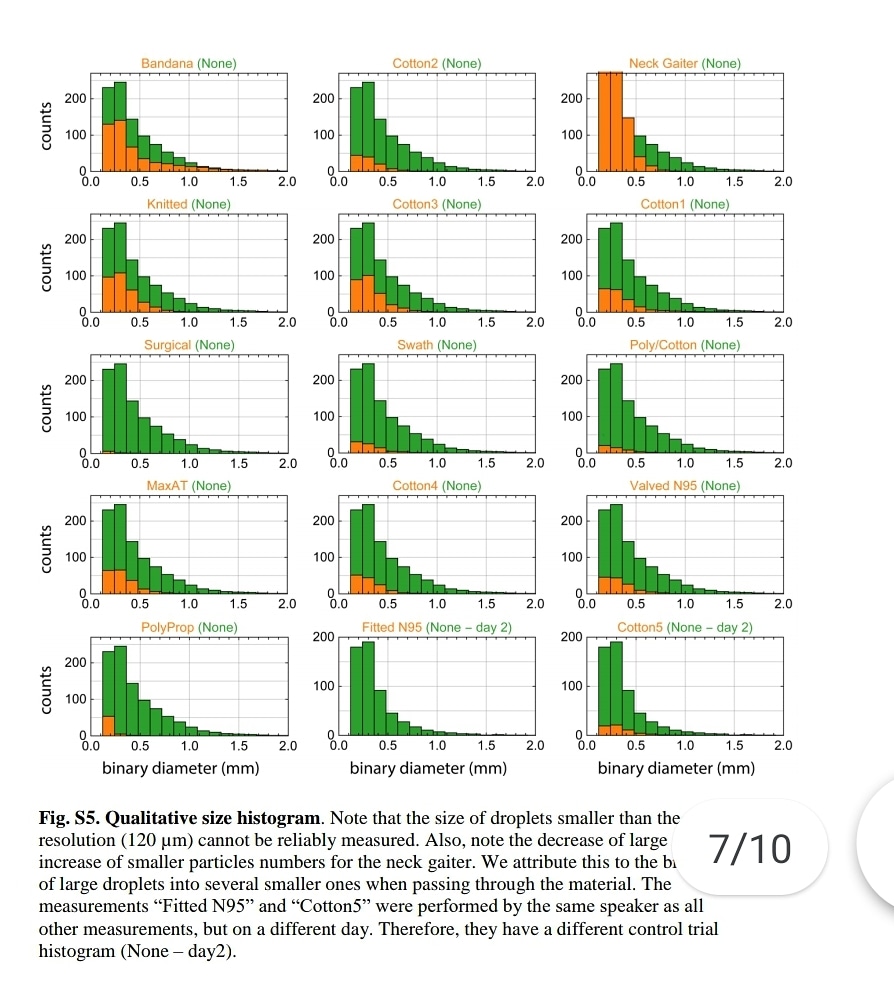
"Speaking through some masks dispersed largest droplets into a multitude of smaller droplets..smaller particles are airborne longer than large droplets (larger droplets sink faster), a mask might be counterproductive."
https://t.co/jBQlWRxcEL
Influenza like illness rates 3 times higher with cloth masks when compared to control group:
https://t.co/djT0mfutv9
Prof. Carl Heneghan, Oxford University: "The high quality trial evidence for cloth masks suggest they increase your rate of reinfection."

Please note, droplets smaller than 120 microns can't be measured. SARSCoV2 is 0.14 microns. This means that the nebulization effect of medical masks could not be measured, not that it does not happen. ⬇️
"Speaking through some masks dispersed largest droplets into a multitude of smaller droplets..smaller particles are airborne longer than large droplets (larger droplets sink faster), a mask might be counterproductive."https://t.co/jBQlWRxcEL pic.twitter.com/XeKYFmjsGs
— Robin Monotti (@robinmonotti) January 15, 2021
The really small aerosols <1 μm [the ones that pass through ALL surgical masks] can penetrate all the way to the alveoli - the basic units for gas exchange
4/In humans, larger aerosols deposit in upper throat, nose, & tracheobronchial region of the lung. Medium-sized aerosols mostly deposit in small airways further down. The really small aerosols <1 \u03bcm can penetrate all the way to the alveoli - the basic units for gas exchange. 4/7 pic.twitter.com/9ZJb4JrZqI
— Dr. Ali Nouri (@AliNouriPhD) December 29, 2020
Here is the Italian-EU scientific study indicating SARSCoV2 replicates in bacteria, not only human cells, and that is why antibiotics work and these vaccines will not:
"The preliminary results suggest that SARS-CoV-2 replicates in bacterial
2 of the 4 authors of the study work at the European Commission. Another works at an Italian medical research facility called Craniomed: https://t.co/EETSM3nb3T
You can find all of CRANIOMED's Carlo Brogna's published scientific research articles here, take a look:
On the 19th March 2020 the WHO released this guidance intended for healthcare workers (HCWs), healthcare managers and IPC teams at the facility level & at national and district/provincial level:https://t.co/C4aV2BnMPj pic.twitter.com/tCk1EyLskV
— Robin Monotti (@robinmonotti) December 21, 2020
It clearly does indicate both the risks of bacterial infection & to prescribe broad spectrum antibiotics as part of treatment:
"Collect blood cultures for bacteria that cause pneumonia and sepsis, ideally before antimicrobial therapy. DO NOT
delay antimicrobial therapy"
"6. Management of severe COVID-19: treatment of co-infections
Give empiric antimicrobials [broad spectrum antibiotics] to treat all likely pathogens causing SARI and sepsis as soon as possible, within 1 hour
of initial assessment for patients with sepsis."
"Empiric antibiotic treatment should be based on the clinical diagnosis (community-acquired
pneumonia, health care-associated pneumonia [if infection was acquired in health care setting] or sepsis), local epidemiology &
susceptibility data, and national treatment guidelines"
"When there is ongoing local circulation of seasonal influenza, empiric therapy with a neuraminidase inhibitor [anti-viral influenza drugs] should
be considered for the treatment for patients with influenza or at risk for severe disease."























